What Does MIPS Stand For in Healthcare?
What is the Purpose of MIPS and How Does it Work?
MIPS Quality Measures
Relationship Between MACRA and MIPS
Using MIPS Successfully
Talk to a Quality Consultant Today
As the world of healthcare continues to evolve, a host of programs and payment models incentivizing improved performance have appeared. One of the most significant of these is the Merit-based Incentive Payment system— or MIPS.
MIPS “reward[s] high-value, high-quality Medicare clinicians with payment increases— while at the same time reducing payments to those clinicians who aren’t meeting performance standards,” according to the Centers for Medicare and Medicaid Services (CMS), the creators of the program.
Many physicians asking “What is MIPS?” are concerned about the downside-risk presented by the program— or, in other words, the possibility of being penalized for not meeting performance standards.
While improving quality performance for healthcare plans and providers under the MIPS evaluative categories is not always straightforward, it is absolutely possible—and can help your organization get as much financial reimbursement as possible.get as much financial reimbursement as possible.
What Does MIPS Mean in Healthcare?
In the context of healthcare, MIPS stands for Merit-based Incentive Payment System. But what exactly is the meaning of MIPS? The Merit-Based Incentive Payment System (MIPS) is program is one of two participation tracks within the CMS’ Quality Payment Program (QPP) that determines Medicare payment adjustments.
MIPS was designed to link payments with high-quality and cost-effective healthcare, ultimately aiming to improve health processes and patient outcomes while reducing the quality of care.
In a nutshell, the QPP seeks to simultaneously reduce the cost and improve the quality of care delivered in the United States. Broadly speaking, it achieves this by incentivizing best practices and penalizing wasteful or redundant actions.The second QPP program is known as Alternative Payment Models, or APMs.
What Are the 4 MIPS Categories?
Any physician, group, or practice manager asking themselves “what is MIPS?” should begin by learning the four scoring categories under which participants of the program are rated. These four categories determine how providers are evaluated to rate their overall performance, and thus reimbursement under the incentive payment plan.
With Performance Year 2022 bringing changes to MIPS that make the program more competitive for providers, it is more important than ever for providers to understand how they are evaluated in these categories.
MIPS Quality Performance
Within the MIPS framework, Quality Performance refers to how well care providers score on a series of metrics aimed at assessing the quality of care delivered. In Performance Year 2022, Quality Performance comprised 30% of an organization’s final MIPS score.
Providers and organizations participating in the merit-based incentive payment system program are able to select six of CMS’ Quality Performance Measures (a full list of the measures can be found here). Providers must then submit data corresponding to these measures for the given performance year to CMS for evaluation.
MIPS Cost Performance
The Cost Performance scoring portion of MIPS is intended to assess providers on their ability to keep cost and spending low. F Beginning in Performance Year 2022, Cost and Quality categories are now rated equally at 30%.
CMS has established 25 different Cost Performance Measures. Once providers have exceeded the established case minimum for each measure, CMS will evaluate their performance. This rating will factor into their final MIPS score.
With the increasingly interconnected nature of healthcare and provider ecosystems, Cost Performance can be one of the trickier categories to manage and score well on, as many factors influencing cost are often out of providers’ control. Still, best practices exist to increase scoring and reimbursement in this area.
MIPS Promoting Interoperability
Promoting Interoperability is a category which primarily refers to Electronic Health Records (EHRs)— as well as other healthcare IT systems— and how well they work together or “interoperate.” As healthcare professionals well know, poorly-integrated systems can lead to inefficient (and more expensive) workflows.
For this reason, CMS created the Promoting Interoperability Performance Category. In Performance Year 2022, this category was worth 25% of a final MIPS score. The stated goal of this category is to enhance “patient engagement and electronic exchange of information using certified electronic health record technology.”
Measures in this category include performance on e-Prescribing, Provider to Patient Exchange, and more.
MIPS Improvement Activities Category
The Improvement Activities Category of the merit-based incentive payment system aims to incentivize physicians to participate in activities that improve their clinical practice. This category was worth 15% of an organization’s final MIPS score in 2022.
A few examples of Improvement Activities measures include Population Management, Care Coordination, and Beneficiary Engagement. The general thinking behind this category is that this incentive, will enhance broader areas of care and and decrease costs.
What is MIPS? The program is complex, and there are many pitfalls— to become a top performer, it pays to understand them. Check out our top 5 MIPS mistakes to avoid here.

What is the Purpose of MIPS and How Does it Work?
According to the Department of Health and Human Services (HHS), CMS “is required by law to implement a quality payment incentive program” which is currently known as the Quality Payment Program. As previously noted, MIPS, along with APM, are the two systems that the CMS uses to measure and reward clinician performance in this program.
With the merit-based incentive payment system, clinicians must report their performance in four MIPS areas: quality, promoting interoperability, improvement activities, and cost. These categories make up the clinicians’ final score, which HHS uses to assess MIPS-eligible clinicians and determine their payment adjustment to Medicare reimbursements every year.
According to HHS, “MIPS was designed to tie payments to quality and cost-efficient care, drive improvement in care processes and health outcomes, increase the use of healthcare information, and reduce the cost of care.”
“MIPS was designed to tie payments to quality and cost-efficient care, drive improvement in care processes and health outcomes, increase the use of healthcare information, and reduce the cost of care.”
MIPS Quality Measures
For the quality category, clinicians are scored based on six MIPS quality measures, which they can select based on what makes the most sense for their practice. CMS releases the final regulations for the Quality Payment Program at the end of every year, which includes the full list of MIPS quality measures.
It is critical that clinicians be aware of any changes to these regulations to ensure they are using current MIPS quality measures that are appropriate for their practice. Failing to do so can have a negative impact on reimbursement.
When evaluating the merit-based incentive payment system quality measures, consider:
- What are the new measures? New quality measures are available for reporting for the first time in that year and do not have historical data for CMS to use for benchmarking. At Medical Advantage, our consultants recommend that practices not use a new measure as one of their top six required measures, since scoring for these new measures will be unpredictable.
- What are the deleted measures? Practices that report a quality measure no longer part of the MIPS reporting program will need to choose a replacement measure.
- What are the topped out measures? Measures with high overall performance rates are capped at seven points, which can impact a clinician’s scoring potential.
- What are the new improvement activities? Clinicians should be aware of improvement activities and how they are weighted, as this can affect their overall scoring potential.
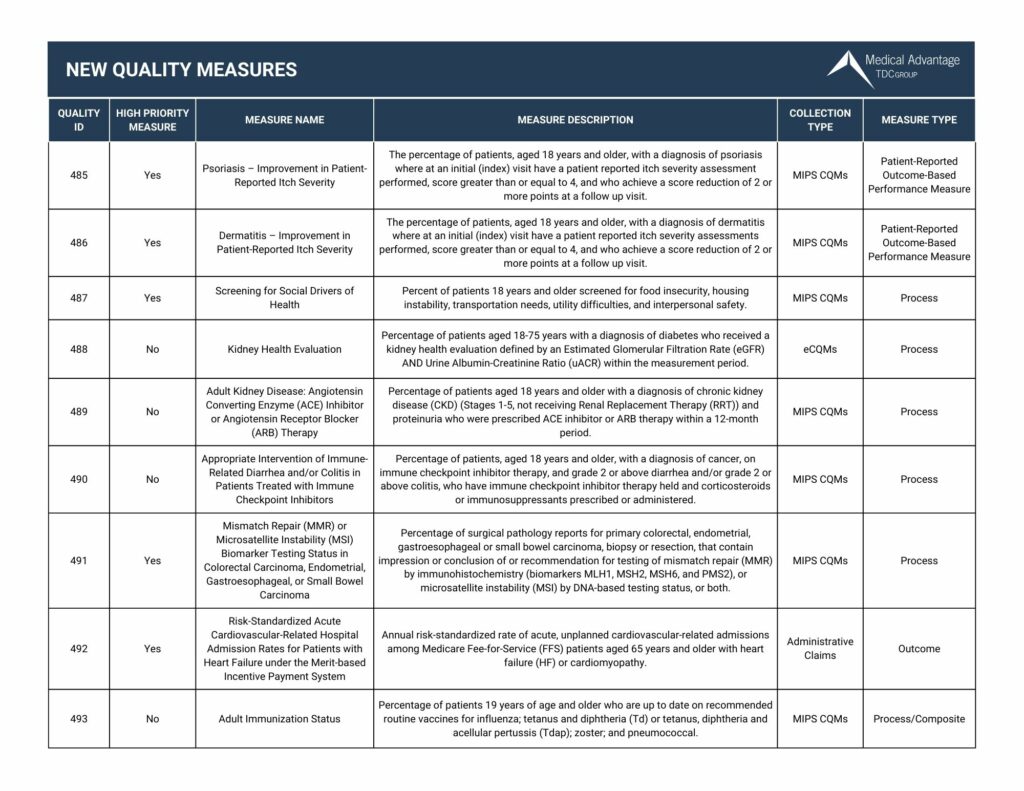
New MIPS Quality Measures for 2023
View our chart below for the new quality measures in 2023. Want to view all the updates for 2023? Click here to download our 2023 Quality Measures Guide
Relationship Between MACRA and MIPS
According to CMS, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is the legislation that created the Quality Payment Program. It streamlined “multiple quality programs” under the new MIPS, and is responsible for changing the way that “Medicare rewards clinicians for value over volume.”
MACRA is significant for any provider of Medicare services because it requires participation in The Quality Payment Program. These providers must measure the quality of their healthcare delivery through one of two tracks: MIPS or APMs. Some companies offer MACRA consulting and support services to help Medicare providers successfully navigate MACRA, maximize incentives, and avoid penalties.
Using MIPS Successfully
Clinicians and practice managers who use MIPS successfully:
- Protect their financial future by increasing incentives and avoiding penalties
- Gain staff buy-in by aligning MIPS goals to what motivates their staff
- Empower a quality champion to provide insight and take the reins on achieving MIPS goals
- Find and use MIPS resources to their advantage
- Optimize their EHR system to support quality measurement
MIPS Consulting Services
If you’re having trouble successfully navigating the MIPS program, you aren’t alone.
“When I was managing my own practice, I spent so much time after hours reading MIPS rules,” says Beth Hickerson, MIPS expert and Medical Advantage’s Senior Consultant for Quality and Healthcare Transformation. “Just understanding MIPS is a full-time job.”
For providers and staff already busy with running a practice and caring for patients, taking time to understand this complex and mammoth piece of healthcare legislation can be daunting.
Luckily, expert MIPS consultants who understand MACRA and industry best practices are here for you. Medical Advantage’s experienced team can guide you through the MIPS process to maximize reimbursement opportunities and avoid penalties, leading to a more efficient and profitable practice.
To learn more about how we can help your organization meet its MIPS goals, contact one of our experts today.





