What is Value-Based Care?
Types of Value-Based Care
What is the Fee-For-Service Care Model?
The Tug of War Between Value-Based Care vs Fee-For-Service
Value-Based Care vs. Fee-For-Service: 5 Key Differences and Benefits
Why Should Your Practice Care?
What’s Next for Fee for Service?
Speak with one of our Healthcare Experts today.
Does your practice utilize the best model for longevity and profitability? Value-based care vs. fee-for-service has been a choice for providers within the last 12 years. Now, in addition to policy shifts deployed by the Centers for Medicare and Medicaid Services CMS, value-based care (VBC) is also being proactively adopted by an increasing number of private payers.
In 2010, the Affordable Care Act (ACA) codified reimbursement for value, or quality, instead of fee-for-service (FFS), or quantity of care. VBC was already emphasized by CMS for the two years prior.
What is Value-Based Care?
Simply put, the VBC Model rewards healthcare providers who focus on the quality of provided care. Reimbursement of services is based on those providers’ effectiveness in preventing illness and promoting health.
Value-based care programs promote better healthcare for individuals, healthier lives for communities, and lower costs over time. Notably, they have been increasingly prominent since the ACA redirected focus toward measuring patient outcomes in contrast to quantifying the care administered without accountability.
Value-based care is focused on providing care that is effective, applied judiciously and documented accurately. Advocates of value-based care vs. fee-for-service say it improves patients’ health and reduces healthcare costs.

The shift to the Value-Based Care Model is expected to continue as the CMS continues to hand down new policies that encourage and incentivize care quality over quantity of encounters.
Types of Value-Based Care
Value-based care can be broken down into four models; the following is a high-level overview of each.
Bundles
In this model, healthcare providers charge a fixed amount for each appointment, regardless of the number of providers who treat the patient. The benefits of the bundled payment system include:
- Greater collaboration.
- Reduced redundant testing.
- Potential cost reduction and improved patient care.
Shared Savings
When using a shared savings model, providers are reimbursed by payers in the same way as fee-for-service models. However, payment is based on quality and spending targets. Advantages of this model include:
- Providers can share savings with the payer when targets are not exceeded.
- If targets are exceeded, providers will not be penalized by the payer.
- Opportunities for providers to partner with Accountable Care Organizations to reduce costs and improve patient care.
Shared Risk
This model, also known as a downside risk model, allows providers to share savings, but not risk, because the provider is accountable to the ACO. Benefits of a shared risk model include an increased potential for profit; however, the risks increase since providers must cover a portion or all the extra costs above target rates.
Global Capitation
As the name alludes, in the global capitation model, providers assume 100% of the risk. Providers are paid a set amount per patient and can keep any savings, but also take on all losses. To reduce risk, providers can use a partial capitation model.
What is the Fee-For-Service Care Model?
The FFS model pays healthcare providers based on individual care services provided, without regard to the effectiveness of that care upon payment.
Despite the ascendant philosophy of value-based care vs. fee-for-service payment model and its continued support under the ACA, the latter remains dominant. A 2020 report by Deloitte Insights notes that 97% of physicians still rely on fee-for-service and/or salary for compensation.
Regarding value-based care: “Yeah, it’s about the evaluations showing that we’re getting better outcomes and lower costs. It’s really about building a better health system. That’s why we got into this in the first place.” – Mark McClellan, MD, PhD, professor at Duke University and founding director of the Duke-Margolis Center for Health Policy
Reasons why fee-for-service remains so entrenched include:
- Legacy claims payment systems are already set up for fee
- Provider support services, including coding and bill preparation, are similarly aligned with legacy systems.
- Legislative and reporting agencies require reports based on units of care that fee-for-service coding systems support.
The Tug of War Between Value-Based Care vs Fee-For-Service
There are also practical reasons behind fee-for-service’s endurance. Two significant barriers are the demand on physicians’ and practices’ time that a shift to value-based care vs. fee-for-service would require, and the immediate need to provide patient care within the existing system.
Beth Hickerson, healthcare consulting expert at Medical Advantage, explains why many have not yet moved to value-based care: “When prioritizing between actual reimbursements now versus theoretical reimbursements at a later date, actual reimbursements will almost always win. This is not because providers are greedy, or even short-sighted. It is because the reimbursement for health care services has not increased to match the cost of inflation. The low reimbursement levels and increased pressure to see as many patients as possible can lead to reactive care patterns. The focus of care changes from what is the best care for each patient to what is the best care that we can provide for this patient in the next 15 minutes.”
Value-Based Care vs. Fee-For-Service: 5 Key Differences and Benefits
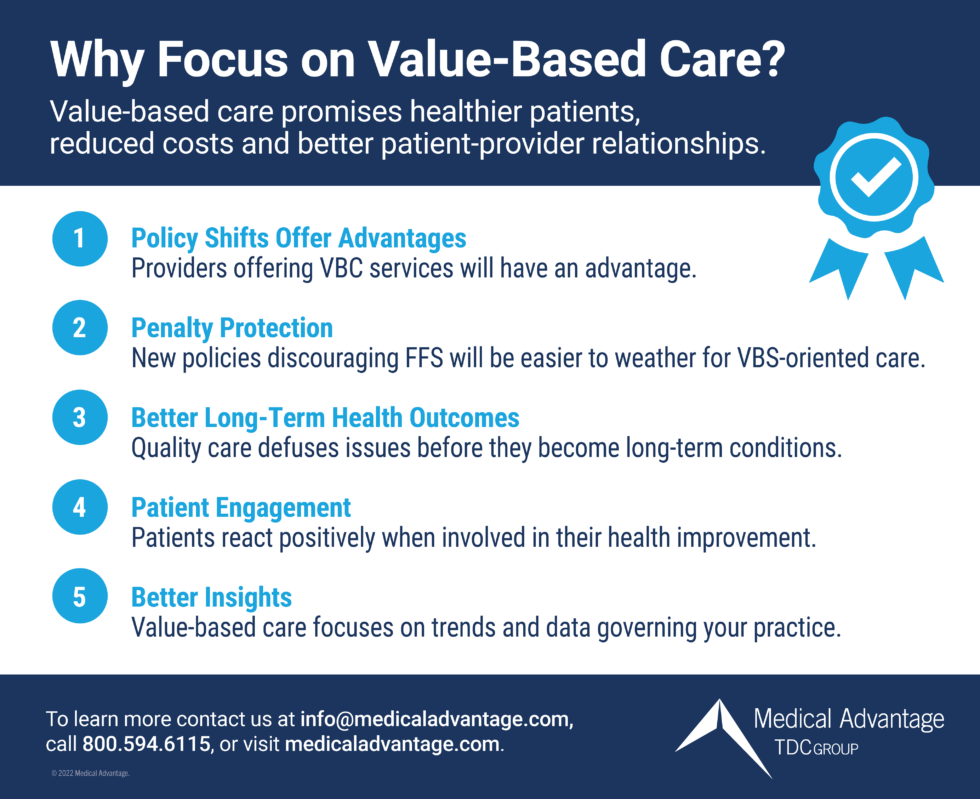
For anyone still wondering what VBC will do for your practice, there are clear benefits:
- Policy shifts offer advantages: As CMS continues to update policy that encourages value-based care, and private payers also shift contracts to account for quality, practices and providers already preparing to offer value-based services will have an advantage over those still focused on fee-for-service.
- Penalty protection: Policies that discourage fee-for-service care will be easier to adopt for a practice or system beginning to adopt value-based reimbursement.
- Better long-term health outcomes: Quality care tends to focus on avoiding issues before they develop into long-term chronic conditions. Your patients will benefit as fewer appointments will focus on dealing with the consequences of avoidable issues.
- Patient engagement: Patients react positively when involved in plans to improve their health. VBC is more cooperative in nature; success requires more patient input, and most are willing to provide it.
- Better insights: Value-based care requires paying closer attention to the trends and data governing your practice and patients. You will learn more about your practice, likely in surprisingly helpful ways.
Why Should Your Practice Care?
Under the ACA’s Medical Loss Ratio (MLR) requirement, systems must spend at least 80 percent of their premium income on healthcare claims and quality of care improvement, leaving the remaining 20 percent for administration, marketing, and profit.
Meanwhile, CMS aims to significantly move healthcare in the country toward value-based care by 2030. More private insurers are taking the initiative to adopt value-based reimbursement.
Between now and then, however, there will be policy changes and new programs that will make proactive value-based care adoption a smart move for practices and organizations.
What’s Next for Fee for Service?
CMS recently proposed a rule that would ensure provider bonuses included as incurred claims in insurers’ medical loss ratios are directly tied to quality or clinical improvement standards, as reported by Modern Healthcare. Also, CMS recommended that only spending directly related to quality improvement should count toward insurers’ quality improvement claims in their ratio.
Accordingly, if finalized, the proposed change directed at insurers/payers could accelerate the adoption of VBC as providers will have to share more information to satisfy the insurers’ MLR requirement under the ACA.
In any event, Value-based care promises healthier patients, reduced costs, and a better understanding between providers and patients. Strong steps in that direction now will pay off with a better positioned practice and healthier clientele.
Medical Advantage Can Help
Shifting to value-based healthcare is daunting, especially for an independent practice. Medical Advantage can help alleviate that burden. Starting with EHR optimization, our consultants can help you document care efficiently and accurately, while ultimately improving VBC performance. We also can work with your staff to train them in best practices for billing and coding in value-based arrangements.
We help practices maximize participation in:
- Accountable Care Organizations
- Merit-Based Incentive Program
- Medicare Shared Savings Program
- Direct Contracting Entities, commercial physician incentive programs, and more.
In fact, we have experience running our own value-based care physician organization, which has seen over $80,000 in shared savings over the past five years! We also support other physicians’ organizations and Accountable Care Organizations to help maximize quality performance and reimbursement for their physicians. To learn more about implementing or optimizing value-based healthcare in your practice, contact one of our consultants today.





