Nearly one million providers participate in Merit-based Incentive Payment System (MIPS), not only to work toward a bonus payment, but also to monitor the care quality of their patients’ population. MIPS is a program offered by the Centers for Medicare & Medicaid Services (CMS) that rewards top performance in preventative care. Staying on top of the changes to CMS quality measurement criteria helps your organization meet your quality goals.
Understanding MIPS Quality Measures
CMS quality measures are standards that healthcare providers use to track and evaluate the quality of care they provide to their patients. By measuring your performance on quality measures, you can assess the degree to which you are meeting the well-established clinical guidelines, standards, and best practices for your specialty, and identify areas where your entire practice may need improvement.
Providers report MIPS chosen measures across a variety of healthcare practice types and situations, including:
- Internal medicine
- Outpatient setting and outpatient office visits
- Multi-specialty practice
The 2023 MIPS quality measures list is typically classified into different categories such as process, outcome, and structural measures. Process measures assess whether patients are receiving appropriate care such as screening, immunizations, and diagnostic tests. Outcome measures assess the effectiveness of treatment by measuring patient outcomes such as mortality, readmission rates, and quality of life. Structural measures assess the practice’s ability to provide quality care, such as care coordination and availability of services.
How do Quality Measures Affect Your Practice?
Quality measures play a significant role in shaping the healthcare landscape. Payers and regulatory authorities, such as the CMS, use quality measures to measure providers’ performance in specific areas to determine eligibility for reimbursement or financial incentives. In a value-based care environment, your quality measure performance can affect your practice’s revenue and sustainability. Some examples include:
- Continuity of Care — Assess how well healthcare providers manage and coordinate their patients’ care, which includes promoting continuity of care through effective communication and information sharing.
- Referrals — Effective care coordination and the exchange of patient information among providers to improve the quality of care provided to patients.
- A recall system — Encouraging patients to come in for routine screenings, follow-up appointments, or preventive care services to help patients receive timely and appropriate care, ensuring patients stay on track with their individual care plans
Additionally, quality measure performance can also influence patient satisfaction and loyalty. Quality measure results are increasingly becoming available to the public, and as patients have increased access to their medical records, they are becoming more conscious of their provider’s quality of care.
By providing high-quality services, you increase your potential to attract and retain more patients as well as increase patient engagement and adherence to clinical guidelines. So, in addition to helping CMS improve the system, your patients and your practice benefit as well.
What’s New for MIPS Quality Measures in 2023?
The changes in MIPS measures for 2023 will significantly impact reimbursement, performance tracking, and workflows of healthcare professionals. Swift response to these changes and their implications can help ensure that your practice thrives and offers the highest quality of care to patients. When preparing for MIPS reporting, consider the following:
- Expansion of eligibility
- Scoring changes
- Updates in quality measures
- Registry submission approach
- Financial implications
1. Quality Measures for 2023
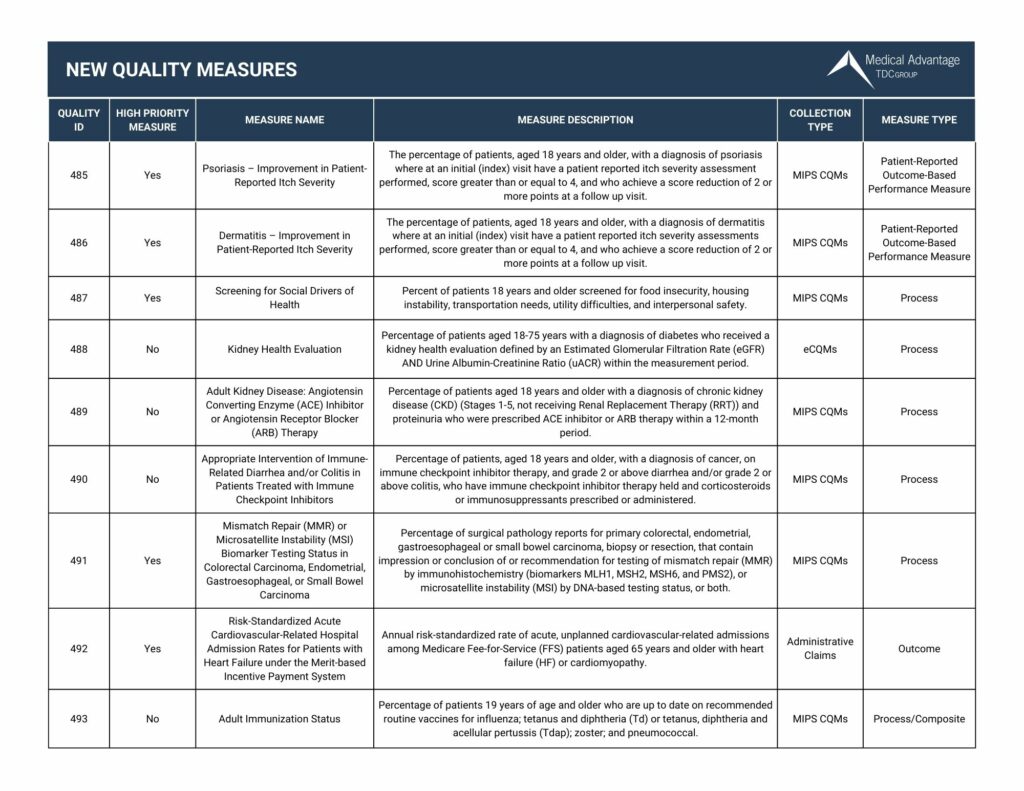
For the first time in 2023, MIPS quality measures are available for reporting. Since these quality measures have not been reported before, historical data from CMS is not currently available for benchmarking.
A clinician or group reporting one of these quality measures will initially earn three points for the measure, assuming the data completeness criteria are met. If enough clinicians or groups report the measure for 2023, CMS may be able to create benchmarks based on performance year data. In that case, reporting clinicians or groups may earn more than three points, depending on performance compared to others who report the measure.
Because scoring for new measures is unpredictable, Medical Advantage’s MIPS consultants recommend that practices report new measures as additional measures – rather than as one of their top six required measures. Keep in mind that because the measures are new, EHR vendors may not have updated the system to reflect measures for 2023 CMS quality public reporting.
2. Deleted Measures: Choosing Replacement Measures
Deleted measures are quality measures that CMS has removed from the MIPS quality reporting program. If a clinician or group reported any deleted measures in 2022 as one of their six required quality measures, they will need to make a replacement measure selection for 2023.
3. Topped-Out Measures: What Clinicians Should Know
Topped-out quality measures have an overall performance rate so high that meaningful performance distinctions and improvements can no longer be made. CMS has a multi-year phase-out cycle for topped-out quality measures. This includes a seven-point cap for measures that have been classified as topped-out for two or more consecutive years.
Clinicians who report a topped-out measure with a seven-point cap will score no more than seven points for that measure, even if they report a perfect performance rate of 100%. For maximum scoring potential, clinicians and groups are encouraged to report topped-out measures with a seven-point cap only as additional measures above the required six measures.
4.MIPS 2023 New Improvement Activities
CMS has added four new Improvement Activities for Year Seven. As a reminder, physicians must achieve a total of 40 points from Improvement Activities during a 90-day reporting period by 50% of their clinicians.
CMS will score activities as either high- or medium-weight. High-weighted activities are worth 20 points, while medium-weighted activities are worth 10 points. Certain clinician types (such as those in small practices) automatically receive double the assigned points for their Improvement Activities.
View our chart below for the new quality measures in 2023. Want to view all the updates for 2023? Click here to download our 2023 Quality Measures Guide
5. MIPS 2023 Deleted Improvement Activities
CMS has removed six Improvement Activities from the list of MIPS quality measures for 2023. Reasons for Improvement Activity removal include reduction of duplicative activities, alignment with current best practice clinical guidelines, meaningful measures initiative, and lack of utilization in prior MIPS reporting years.
How Are Quality Measures Scored?
Each MIPS Quality Measure has a score ranging from 0 to 10 points, with the maximum score being 10. The score is based on the provider’s performance compared to the benchmark set by the CMS. The benchmark is derived from the performance data submitted by other providers who reported the same Quality Measure. The scoring method is designed to be fair, so even if providers’ overall scores vary, they are still graded against a standard that considers their patients’ diagnosis, severity of illness, and other factors.
How are Individual Measure Scores Calculated?
At the individual level, Measure Scores are calculated by dividing the number of points earned by the maximum possible points. A measure’s maximum score can vary based on whether the provider submitted data for the measure. The score is calculated for each individual measure and added together to get the provider’s Total Quality Score.
Weighting of Quality Scores
CMS assigns a weight to each of the four performance categories: Quality, Cost, Promoting Interoperability, and Improvement Activities. The Quality category weight is 45% of the total MIPS score. The Cost category is 15%, with the Promoting Interoperability and Improvement Activities weighing 25% and 15%, respectively.
How Quality Scores Affect Payments
The Total Quality Score determines the provider’s Medicare Part B payment adjustment. That adjustment is a percentage increase or decrease in Medicare Part B reimbursements based on the provider’s performance compared to his or her peers. The adjustment is related to the provider’s payment year; so, if the provider has a successful year, the adjustment for the next year increases.
How Practices Should Report on Quality Measures
CMS provides a list of measures appropriate for different specialties to help providers choose the measures that best fit their practice. Some examples of different quality measures for specialties include:
- Dermatology
- Tobacco use
- Cardiology and coronary artery disease
- Social work
- Internist
Once the appropriate MIPS quality measures have been selected, the next step is to collect accurate data for each measure. There are various sources that can be used to collect and report this data. Electronic Health Record (EHR) systems are utilized to collect the data and produce reports that show how the practice performed on each measure.
Other sources of data may include claims data, registries, or patient surveys. To have a clear and accurate idea of where the practice stands on scoring, it is important for healthcare professionals to ensure that they are using the appropriate data sources for each MIPS quality measure.
Monitoring Progress and Identifying Areas for Improvement
After collecting accurate data, it is important for healthcare professionals to monitor their progress and identify areas for improvement. This can be accomplished by comparing current performance to past performance and to performance levels of other practices – also known as benchmarking. By doing so, healthcare professionals can identify areas where they need to improve and adjust their processes accordingly.
Submitting Data on Time
Finally, it is important for healthcare professionals to submit MIPS quality measure data on time. Failure to submit data on time can result in a penalty, which can impact reimbursement rates for the practice, meaning the team does not get credit for all their hard work Deadlines for submission can vary based on the reporting option chosen and can be checked on the CMS website.
Implementing Best Practices for Reporting
Overall, healthcare professionals should implement several best practices for proper reporting of MIPS quality measures. This includes understanding the measures, collecting accurate data, monitoring progress, and submitting data on time. By doing so, healthcare professionals can ensure that their practice gets a favorable score by meeting requirements, improving patient outcomes, and avoiding penalties.
How Do Healthcare Consultants Help with CMS Quality Measures?
With MACRA constantly changing from year to year, it can be challenging for practices to keep up with the quality payment program. Now is the perfect time to consider partnering with CMS experts like Medical Advantage’s MIPS consultants for personalized one-on-one support. Our MIPS consultants have years of experience working as practice managers, nurses, and billing specialists.
Medical Advantage also invites providers to join our accountable care organization (ACO) for comprehensive support with a variety of quality initiatives including MIPS. Get in touch today for a free consultation to find out how our services can support your practice and continue improving quality of care.





