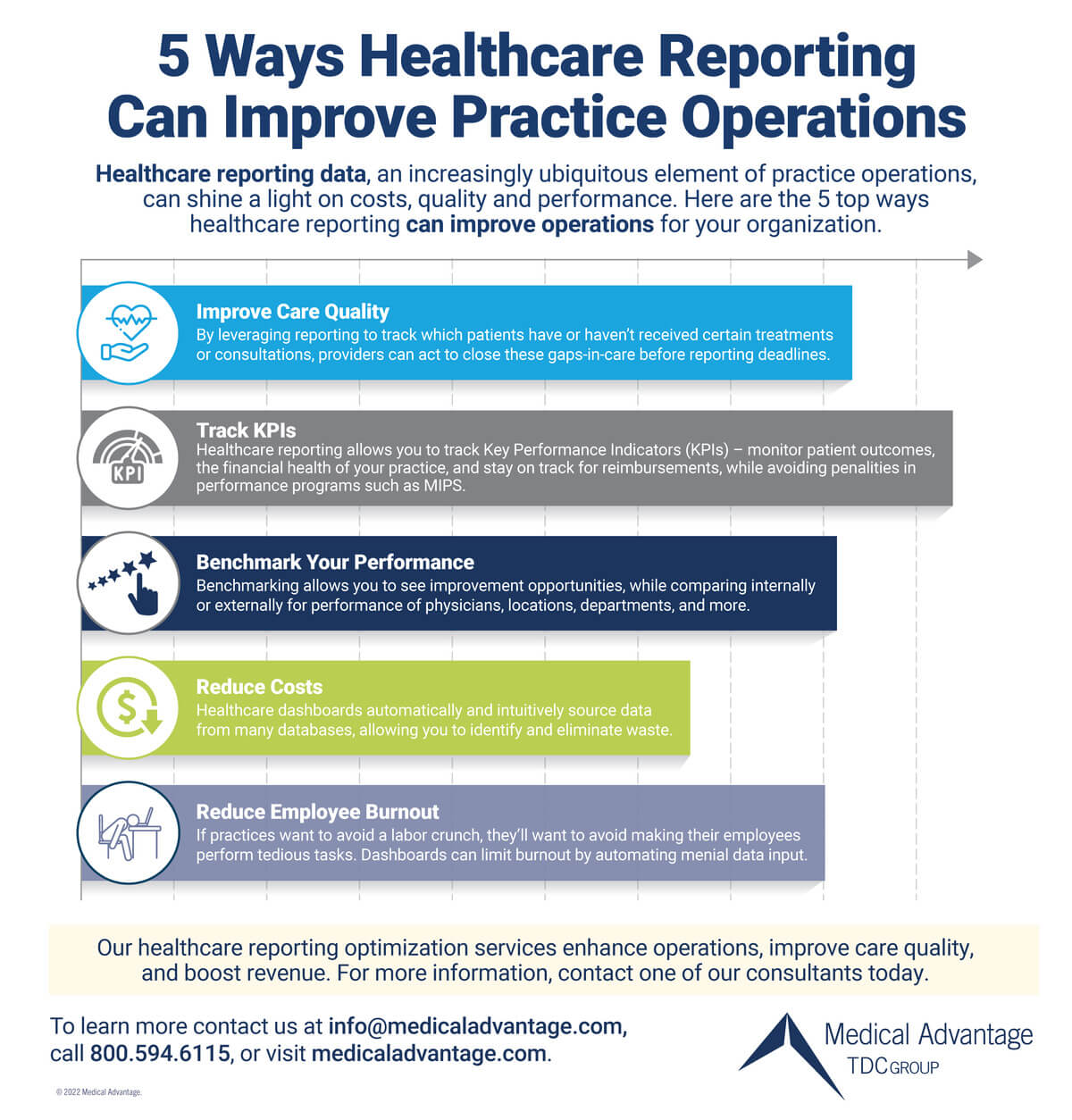
Data is abundant in the digital age; thus, adequate healthcare reporting is becoming more necessary. When done effectively, healthcare reporting – a term that refers to turning raw data into useful insights and reports – can improve patient outcomes and revenue while reducing costs, as well as demand for human resources.
Adverse issues can arise when a healthcare organization’s IT and reporting systems are not effectively designed and managed. Common problems caused by inadequate and inefficient healthcare reporting are:
- Reduced reimbursements
- Increased penalties from payers
- Poor patient outcomes
- Wasteful spending
- Erroneous decision-making regarding the business
- Staff and employee burnout
To help your healthcare group navigate pitfalls and maximize the benefits of its reporting infrastructure, we have gathered some top tips and best practices based on decades’ worth of experience assisting and providing solutions to clients.
Healthcare Reporting: Why It is Important
The compiling of reports and tracking of key performance indicators (KPIs) is common for nearly all industries, and healthcare is no exception. However, for organizations – in the healthcare domain in particular – reporting and KPIs are even more crucial. Reporting is one of the most important ways to view and track whether patient outcomes are auspicious, and if the organization is financially sound. Healthcare reporting is also a means of earning reimbursements and avoiding penalties in the case of groups under value-based care contracts.
In a very broad stroke, reporting is moving from the raw data an organization creates to more useful information. This can include a database management system consisting of a data warehouse on the back end along with a BI (or business intelligence) solution on the front-end – this is commonly accomplished with a variety of tech stacks.
Empowered by readouts and oversight of their data, and performance in numerous areas, organizations are properly equipped to observe, analyze, and act upon where they are over- and underperforming.
“Effective reporting helps cut down on waste spending in healthcare. It helps address overtreatment, low-quality care, failed care coordination, failed care delivery, and more. All these things add cost,” says Linda Yang, IT Business Consultant with Medical Advantage. “Good reporting can help make these issues more visible, empowering providers address them – both increasing care quality and reducing cost in the process.”
Challenges to Effective Healthcare Reporting
It goes without saying that the main goal of healthcare organizations is to provide accessible, quality care at a reasonable price – but enter IT and other forms of technology and this can be easier said than done.
Healthcare personnel may initially lack expertise or training to effectively manage in-house databases and software. Further, organizations that continue to use manual or paper-based methods for reporting and data management often struggle with higher employee workload, redundant workflows, and increased capital expenditure. Both of these issues present challenges that organizations must overcome when implementing effective strategies.
Another issue medical practices, hospitals, and organizations must contend with when building viable reporting workflows is the sheer complexity, volume, and sensitivity of data in modern healthcare. Not only is healthcare data often generated in large quantities, but much of it also falls under HIPAA- standards and is quite sensitive in the context of patient privacy. For this reason, databases must not only be scalable and elastic enough to handle complex and copious amounts of data, but they must also be secure to guard against potential network breaches while ensuring data integrity.
Fragmentation is the third and final challenge to healthcare reporting. Healthcare data is often found in various formats and in disparate locations – think data acquired via EHRs (Electronic Health Records Systems), financial software, ERMs, HR (Human Resources) software, patient intake platforms, etc. Acquiring and integrating this data into one report is a hurdle that organizations of all sizes must overcome. Often, outsourcing healthcare data management via solutions such as healthcare dashboards can automate and simplify this process.
Best Practices in Healthcare Reporting
Overcoming challenges to effective reporting can be made much easier by following experience-based best practices. By doing so, your organization can improve its reporting prowess – both increasing care quality and reducing costs in the process.
Choosing Which Key Performance Indicators to Track
When choosing which healthcare KPIs (Key Performance Indicators) to track, an organization has an abundance of options. A host of clinical, operational, financial, and other types of data are available to be tracked. It all depends on the specific goals of the organization.
For example, a private equity group with an eye on a specific practice may be interested in measuring and tracking return on investment or other financial metrics. In this case, financial KPIs (gross revenue, revenue drivers, staffing costs, overall cost per service, charges, and more) would be prioritized.
To offer another example, the leadership of a medical practice could have an overall goal of improving patient care, especially if there are existing value-based care contracts. To that end, KPIs such as procedures and tests performed, population health statistics, and other data concerning gaps in care would be of the utmost importance.
In general, KPIs can be virtually anything – any metrics a group, practice, or healthcare entity is wanting to track. Whatever clinical, operational, financial, or business issues an organization is looking to solve, a KPIs can be defined and monitored to help do just that.
Close Gaps in Care
As healthcare continues to transition to a value-based care model, payers are more interested than ever in how well practices are closing gaps in care and reducing costs. One of the major reasons for this is that reimbursements (and penalties) are increasingly being tied to performance across various quality metrics as well as patient outcomes.
One of the best ways to close gaps in care is with healthcare reporting. By tracking which patients have or haven’t received certain treatments or consultations, providers can act swiftly to reach out and close these gaps in care before reporting deadlines.
Of course, not only does this help improve reimbursement from payers, but it will also help improve patient outcomes. Better data on how your patients are doing helps providers and practice leadership make better decisions. If the trends are going in the wrong direction – say, increased emergency department visits or readmission rates – leadership can intervene and help mitigate such trends. Ultimately, being more proactive and utilizing these preventative care strategies help reduce costs.
Benchmark Your Performance
In general, benchmarking is the comparison of the performance of a subset of a group to overall group performance, whether this performance be measured in group averages, percentiles, etc. Across the vast landscape of healthcare in the United States, there is a vast array of benchmarks relevant to all kinds of local and national groups of healthcare organizations, practice groups, ACOs (Accountable Care Organizations), etc.
The CMS (Centers for Medicare & Medicaid Services) has its own set of benchmarks, but there are many private data aggregators who have access to CMS claims data as well as data from private payors, and these benchmarks –as well as source data – are made available to practice groups interested in benchmarking their own performance against their peers.
A proper data management system should always incorporate benchmarks where possible in the interest of establishing a reliable “yardstick” of sorts with which to compare their performance. At Medical Advantage, our benchmarks are powered by CareJourney, but there are several different data aggregators with which healthcare organizations can consult with respect to benchmarks. Ideally, these benchmarks are incorporated into the organization’s data warehouse and added to front end visualizations in order to help organizations establish performance objectives.
Integrate Data Across Systems
As mentioned above, fragmentation is a widespread issue in healthcare. In the context of data management, this means myriad data in so many different formats and locations. Thus, it is imperative that data be centralized and integrated before any meaningful analysis can take place. Integrating all this information into a data warehouse to provide a single source of truth and allow the use of a business intelligence front end is a crucial first step in properly using organizational data.
Enter healthcare reporting with dashboards. Healthcare dashboards automatically, securely, and efficiently source data from many different operational databases (to name a few: EHR, HR, marketing CRMs, patient intake software, accounting software, scheduling software, website metrics, and more) into one central, dynamic report that allows interactive data slicing and drill down.
The purpose of this is to discover insights that can only be gleaned when all the data is integrated in a single repository. For example, if revenue is down, it may be difficult to ascertain why – until you employ a comparative analysis between locations, providers, and payers, etc., to properly evaluate various metrics. Dashboards help ensure a holistic, integrated view, which allows you to bring all data and insights within the purview of management and other stakeholders.
Preserve Human and Financial Resources
The healthcare labor market is under pressure – there is a lot of burnout, employment mobility, and a widespread willingness on the part of employees to leave their jobs. Menial, frustrating, and unfulfilling tasks are a large contributor to this sentiment. If practices want to avoid a labor crunch, they will also want to avoid making their employees perform tedious and banal tasks. Dashboards can help reduce that.
For one, implementing a solution that automates data management (such as healthcare dashboards) eliminates the need for employees to tediously hand-produce reports every month, week, or even day. In addition, not only does this automated process reduce the need for human resources, but it also eliminates the need for on-prem computing resources, software licenses, and data storage as services are moved to the cloud.
Cloud-based data management services are more cost-effective in the long run. What’s more, these systems are highly scalable, meaning if your organization and its data are expanding, the data management services can easily keep up.
Healthcare reporting and effective data management – particularly when done via cloud-based services – is an excellent way to preserve human and financial resources, not only saving your organization money but also mitigating employee dissatisfaction.
Medical Advantage Can Help
Modern healthcare dashboards – like the ones facilitated by the experienced medical experts at Medical Advantage – enable large practices, private equity groups, health plans, hospitals, and more to get the most out of their healthcare reporting. Optimization via our dashboard solution also streamlines operations, improves care quality, and boosts revenue. For more information, contact one of our consultants today.





